The Warning Signs of Acid Reflux: What You Need To Know
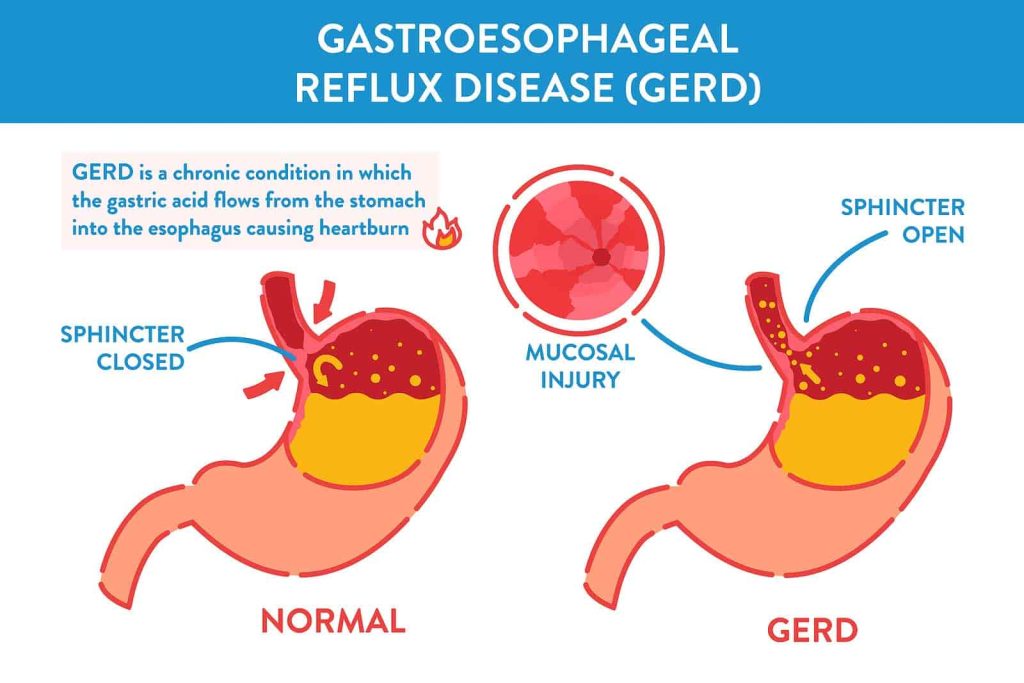
Acid reflux, also known as gastroesophageal reflux (GER), occurs when stomach acid flows back into the esophagus, causing irritation and discomfort. This common condition affects millions of people annually, with over 20% of Americans experiencing symptoms at least weekly. Recognizing its warning signs early can help in managing and preventing complications.
How to Recognize If You Have Acid Reflux
Knowing how to identify the warning signs is crucial for managing the condition and preventing long-term complications. The most common symptom is heartburn – a burning sensation in the chest or throat, often worse after eating or lying down. Some individuals also experience regurgitation, where stomach acid or partially digested food comes back into the mouth, leaving a sour taste. Other signs include difficulty swallowing, chronic sore throat, or a feeling of a lump in the throat. Less obvious symptoms may include persistent coughing, wheezing, or dental erosion caused by acid exposure.
- Acid reflux can be triggered by eating large meals, consuming acidic or fatty foods, smoking, or being overweight. Recognizing your specific triggers is key to controlling symptoms.
- If you suspect you have acid reflux, monitoring these symptoms and consulting a healthcare professional is essential. They can confirm the diagnosis and recommend treatments such as dietary changes, medications, or other interventions to reduce acid production and protect the esophagus.
- Being proactive about addressing acid reflux can prevent complications like esophagitis or even precancerous changes in the esophagus, making early recognition critical for long-term health.
Can I Manage It Without Medication?
While medications can help, many individuals wonder if lifestyle changes alone can manage symptoms effectively. The answer depends on recognizing your triggers and making targeted adjustments to your daily habits.
- Start with Your Diet. One of the most impactful changes is altering your diet. Certain foods, like spicy dishes, fatty meals, citrus fruits, chocolate, and caffeine, are common triggers for acid reflux. Reducing or eliminating these foods from your diet can significantly decrease the frequency and severity of symptoms. Smaller, more frequent meals instead of large portions can also help by minimizing pressure on the stomach.
- Adjust How and When You Eat. Timing matters as much as the food itself. Avoid lying down or reclining for at least two to three hours after eating, as this can increase the likelihood of acid reflux. Elevating the head of your bed by 6-8 inches can also reduce nighttime symptoms by keeping stomach acid from traveling upward.
- Maintain a Healthy Weight. Carrying excess weight, especially around the abdomen, can increase pressure on the stomach, making acid reflux worse. Studies show that even a 10% reduction in body weight can lead to significant improvements in symptoms. Regular physical activity and a balanced diet are essential components of managing weight effectively.
- Eliminate Harmful Habits. Smoking weakens the lower esophageal sphincter (LES), the muscle that prevents stomach acid from rising into the esophagus. Quitting smoking not only benefits overall health but also reduces the risk of acid reflux. Alcohol consumption can also relax the LES and irritate the stomach lining, so reducing or eliminating alcohol intake is advisable.
- Monitor and Adjust. Lifestyle changes require consistency and attention to detail. Keep a symptom journal to identify what triggers your acid reflux and adjust accordingly. If symptoms persist or worsen despite these measures, consulting a healthcare professional is essential.
What Medications Can Be Used for Treatment?
Depending on the severity of symptoms, treatment options range from over-the-counter remedies to prescription medications. Here’s a comprehensive look at the types of drugs commonly used for acid reflux and how they work. Medications for acid reflux, including PPIs, H2 blockers, and antacids, are available through a certified Canadian online pharmacy with international delivery options, at lower prices compared to other markets. For example, generic Esomeprazole can cost as little as $0.30 per pill when purchased in bulk, providing an affordable solution for long-term treatment. You can also use an online service such as GoodRx, which will help you find the most affordable and accessible options in the United States.
Antacids. Antacids are often the first line of defense against acid reflux. These medications work by neutralizing stomach acid and providing quick relief from symptoms like heartburn. Commonly used antacids include:
- Calcium Carbonate (Tums)
- Magnesium Hydroxide (Milk of Magnesia)
- Aluminum Hydroxide (Maalox)
While effective for occasional symptoms, antacids do not address the underlying causes of acid reflux and are not suitable for long-term use.
H2 Receptor Blockers. H2 receptor blockers reduce acid production in the stomach by targeting histamine receptors. They are typically used for mild to moderate symptoms and provide relief that lasts longer than antacids. Examples include:
- Ranitidine (Zantac)
- Famotidine (Pepcid)
These medications can be purchased over-the-counter or in higher doses with a prescription.
Proton Pump Inhibitors (PPIs). Proton Pump Inhibitors are considered one of the most effective treatments for moderate to severe acid reflux. They block acid production at the source by inhibiting the enzyme responsible for acid secretion. Common PPIs include:
- Omeprazole (Prilosec)
- Esomeprazole (Nexium)
- Pantoprazole (Protonix)
PPIs are often prescribed for long-term use to manage chronic GERD or heal damage to the esophagus caused by prolonged acid exposure.
Prokinetic Agents. For individuals whose reflux is caused by delayed stomach emptying or motility issues, prokinetic agents like Metoclopramide (Reglan) may be prescribed. These medications enhance stomach contractions to speed up the emptying process, reducing the likelihood of acid backing up into the esophagus.
When choosing treatment for acid reflux, consulting a healthcare provider is essential to ensure the selected medication is appropriate for your specific symptoms and needs.
When Should You See a Doctor?
Acid reflux, or gastroesophageal reflux disease (GERD) when chronic, can usually be managed with lifestyle changes or over-the-counter medications. However, there are certain situations where medical attention is not just advisable but essential to prevent serious complications. Recognizing these signs early can make all the difference.
Persistent Symptoms Despite Treatment
If acid reflux symptoms such as heartburn, regurgitation, or chest discomfort persist despite dietary adjustments, weight management, and the use of antacids or other medications, it’s time to consult a healthcare professional. Persistent symptoms may indicate underlying conditions, such as a hiatal hernia or severe GERD, requiring specialized treatment.
- Difficulty Swallowing. Experiencing difficulty or pain while swallowing, known as dysphagia, could signal esophageal narrowing or damage from prolonged acid exposure. This symptom should never be ignored, as it may also point to more serious issues like esophageal strictures or Barrett’s esophagus, both of which warrant immediate medical evaluation.
- Unexplained Weight Loss. Unintended weight loss in the context of acid reflux may indicate a more severe condition affecting the digestive system, such as an esophageal ulcer or even early stages of esophageal cancer. A thorough examination is crucial to determine the cause and initiate appropriate intervention.
- Chronic Cough or Respiratory Issues. When acid reflux leads to frequent coughing, wheezing, or other respiratory problems, it could be a sign that stomach acid is reaching the upper airway. Known as laryngopharyngeal reflux (LPR), this condition can damage the vocal cords and throat, necessitating prompt medical attention.
- Signs of Bleeding. If you notice black, tarry stools or vomit that resembles coffee grounds, these could be symptoms of gastrointestinal bleeding caused by severe esophagitis or an ulcer. These signs require immediate emergency care.
About Dr. Thomas
Dr. Thomas has been a partner physician with AMG since 1990. He manages the implementation of compliance policies and procedures and ensures corporate compliance with federal, state and local policies. Dr. Thomas has served in many leadership positions, including Chief of Anesthesiology at St. Thomas Hospital from 1992 to 2000, medical director of St. Thomas Surgicare (an outpatient surgery center) from 2002 to the present and member of the AMG Board of Directors from 1996 to 2012.
